Introduction
a. Understanding Psoriatic Arthritis
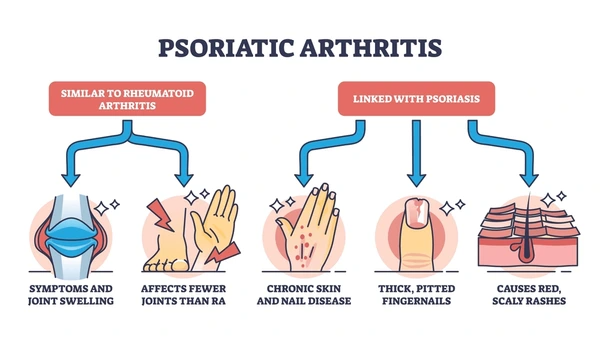
Psoriatic arthritis (PsA) is a chronic autoimmune condition that combines the symptoms of arthritis and psoriasis. It affects the joints and skin, leading to inflammation, pain, stiffness, and scaly patches. While psoriasis usually precedes the onset of arthritis, PsA can develop at any stage of life and can affect different joints, including the fingers, toes, and spine.
The exact cause of PsA is not fully understood, but it is believed to involve a combination of genetic, environmental, and immune system factors. This complex condition can significantly impact the quality of life, making daily activities challenging and leading to fatigue and depression if not managed effectively.
b. The Role of Diet in Managing Psoriatic Arthritis
Diet plays a vital role in managing chronic inflammatory conditions like Psoriatic arthritis. While no specific diet can cure PsA, certain foods can help reduce inflammation, support overall health, and potentially minimize flare-ups. Conversely, some foods may exacerbate inflammation and worsen symptoms.
Adopting a balanced, anti-inflammatory diet can be a key component of a comprehensive treatment plan for PsA. By understanding which foods to include and which to avoid, individuals with PsA can take proactive steps to manage their condition more effectively.
c. Overview of the Article’s Content
This article will delve into the connection between diet and Psoriatic arthritis, providing detailed insights into the foods that can help manage the condition and those that should be limited or avoided. We will explore the benefits of the Mediterranean diet, offer practical meal planning tips, and highlight the importance of specific nutrients. Additionally, expert insights and recent research findings will be discussed, followed by a look at future trends in diet and PsA management.
The Connection Between Diet and Inflammation
a. How Diet Influences Inflammation
Inflammation is a natural response by the immune system to protect the body from injury and infection. However, in autoimmune conditions like PsA, the immune system mistakenly attacks healthy tissues, leading to chronic inflammation. Diet can either contribute to or help mitigate this inflammatory response.
Certain foods, particularly those high in saturated fats, refined sugars, and artificial additives, can trigger the release of inflammatory markers such as cytokines. These markers can exacerbate joint pain, swelling, and other symptoms associated with PsA. On the other hand, foods rich in antioxidants, omega-3 fatty acids, and fiber have been shown to reduce inflammation by neutralizing free radicals, supporting immune function, and promoting a healthy gut microbiome.
b. Inflammation and Psoriatic Arthritis
In Psoriatic arthritis, inflammation is not confined to the joints but can also affect the skin, cardiovascular system, and other organs. Chronic inflammation can lead to complications such as increased risk of heart disease, metabolic syndrome, and even mental health issues like depression.
Managing inflammation through diet is crucial for preventing these complications and maintaining overall health. By reducing the intake of pro-inflammatory foods and increasing anti-inflammatory nutrients, individuals with PsA can help control their symptoms and improve their quality of life.
Foods to Include in Your Diet
a. Anti-Inflammatory Foods
Anti-inflammatory foods are rich in nutrients that combat oxidative stress and support immune function. These include:
- Berries: Blueberries, strawberries, and raspberries are packed with antioxidants, particularly anthocyanins, which have been shown to reduce inflammation.
- Leafy Greens: Spinach, kale, and Swiss chard are excellent sources of vitamins A, C, and K, as well as fiber, which all contribute to reducing inflammation.
- Nuts and Seeds: Almonds, walnuts, and flaxseeds provide healthy fats, fiber, and antioxidants that support heart health and reduce inflammation.
Including a variety of these foods in your diet can help provide a broad spectrum of nutrients that work synergistically to combat inflammation.
b. Omega-3 Rich Foods
Omega-3 fatty acids are well-known for their anti-inflammatory properties and are particularly beneficial for those with PsA. These essential fats can be found in:
- Fatty Fish: Salmon, mackerel, sardines, and tuna are rich in omega-3 fatty acids, which help reduce the production of inflammatory molecules.
- Flaxseeds and Chia Seeds: These plant-based sources of omega-3s are easy to add to smoothies, salads, and yogurt.
- Walnuts: In addition to omega-3s, walnuts provide antioxidants and polyphenols that contribute to overall inflammation control.
Regular consumption of omega-3-rich foods can help decrease joint pain and stiffness, making them a valuable part of a PsA-friendly diet.
c. Fruits and Vegetables
A diet rich in fruits and vegetables provides essential vitamins, minerals, and antioxidants that support overall health and reduce inflammation. Some key examples include:
- Berries: Blueberries, strawberries, and raspberries are high in antioxidants, particularly anthocyanins, which have anti-inflammatory effects.
- Citrus Fruits: Oranges, grapefruits, and lemons are rich in vitamin C, an antioxidant that helps reduce inflammation and supports immune function.
- Cruciferous Vegetables: Broccoli, cauliflower, and Brussels sprouts contain sulforaphane, a compound that has been shown to block inflammatory pathways.
Eating a wide variety of fruits and vegetables ensures that you get a diverse range of nutrients that support immune health and help keep inflammation at bay.
d. Whole Grains
Whole grains are an important part of an anti-inflammatory diet due to their high fiber content and low glycemic index. Examples include:
- Brown Rice: A versatile whole grain that can be used in a variety of dishes, providing fiber, B vitamins, and minerals.
- Quinoa: A gluten-free grain that is high in protein and essential amino acids, making it a great addition to salads, bowls, and side dishes.
- Oatmeal: A heart-healthy option that provides soluble fiber, which helps reduce cholesterol levels and support digestive health.
Whole grains help maintain steady blood sugar levels, reducing the risk of inflammation and associated flare-ups.
e. Lean Proteins
Protein is essential for muscle repair, immune function, and overall health. Lean protein sources that are low in saturated fats include:
- Chicken and Turkey: Skinless poultry provides high-quality protein without the added saturated fats that can contribute to inflammation.
- Tofu and Tempeh: These plant-based protein options are rich in nutrients and can be used in a variety of dishes, from stir-fries to salads.
- Legumes: Beans, lentils, and chickpeas are excellent sources of plant-based protein and fiber, supporting both muscle health and digestive function.
Choosing lean proteins helps ensure that you get the necessary nutrients without increasing your intake of pro-inflammatory fats.
f. Probiotics and Fermented Foods
Gut health is closely linked to immune function and inflammation. Probiotic-rich foods can help maintain a healthy gut microbiome, which in turn supports overall health. Some examples include:
- Yogurt and Kefir: These fermented dairy products are rich in probiotics that support digestive health and help regulate the immune system.
- Sauerkraut and Kimchi: Fermented vegetables that provide beneficial bacteria and enzymes that promote gut health and reduce inflammation.
- Miso and Tempeh: Fermented soy products that are rich in probiotics and can be used in a variety of savory dishes.
Incorporating fermented foods into your diet can help support a healthy gut, which is crucial for managing inflammation and PsA symptoms.
Foods to Avoid or Limit

a. Processed and Red Meats
Processed meats, such as bacon, sausages, and deli meats, as well as red meats like beef and lamb, are high in saturated fats and advanced glycation end products (AGEs), which can increase inflammation. Limiting these foods is important for managing PsA.
- Processed Meats: These are often high in sodium, preservatives, and saturated fats, all of which can contribute to increased inflammation and heart disease risk.
- Red Meats: While red meats provide protein and iron, they can also increase the levels of inflammatory markers in the body. Opt for lean cuts or plant-based alternatives when possible.
Reducing your intake of processed and red meats can help lower your risk of inflammation-related complications.
b. Refined Carbohydrates and Sugars
Refined carbohydrates and sugars, found in white bread, pastries, and sugary drinks, can lead to spikes in blood sugar levels and increase inflammation. These foods are best avoided or consumed in moderation.
- White Bread and Pastries: These refined grains have been stripped of fiber and nutrients, leading to quick spikes in blood sugar that can trigger inflammatory responses.
- Sugary Drinks: Sodas, energy drinks, and sweetened teas are high in added sugars, which contribute to chronic inflammation and can worsen PsA symptoms.
Replacing refined carbs and sugars with whole grains and naturally sweet foods like fruits can help manage blood sugar levels and reduce inflammation.
c. Dairy Products
Dairy products can be inflammatory for some people, especially those with lactose intolerance or sensitivity. If you notice that dairy exacerbates your PsA symptoms, consider reducing your intake or trying plant-based alternatives.
- Milk and Cheese: These dairy products are common sources of saturated fats and can be inflammatory for some individuals.
- Plant-Based Alternatives: Almond milk, soy yogurt, and coconut-based products are great dairy-free options that provide similar textures and flavors without the inflammation risk.
Experimenting with dairy alternatives can help you identify whether dairy is a trigger for your symptoms.
d. Alcohol
Alcohol can contribute to inflammation and may interfere with medications used to treat PsA. Limiting alcohol consumption or avoiding it altogether is advisable for those managing PsA.
- Alcohol: Alcoholic beverages can increase inflammation and interfere with the effectiveness of certain medications used to treat PsA. Excessive alcohol consumption is also linked to a higher risk of cardiovascular disease, which PsA patients are already at increased risk for.
Choosing non-alcoholic alternatives or drinking alcohol in moderation can help reduce inflammation and avoid potential complications.
e. Nightshade Vegetables
Nightshade vegetables, such as tomatoes, potatoes, peppers, and eggplants, contain solanine, a compound that may contribute to inflammation in some individuals with PsA. While not everyone is sensitive to nightshades, it may be worth experimenting with eliminating them from your diet to see if symptoms improve.
- Tomatoes: Rich in vitamins A and C, but may cause inflammation in sensitive individuals.
- Potatoes and Peppers: Commonly used in various dishes but may need to be limited if you notice an increase in joint pain after consuming them.
If you suspect nightshade vegetables are affecting your symptoms, consider eliminating them for a few weeks and then reintroducing them to observe any changes in your condition.
The Mediterranean Diet and Psoriatic Arthritis

a. Overview of the Mediterranean Diet
The Mediterranean diet is renowned for its heart-healthy and anti-inflammatory properties, making it an ideal choice for those with Psoriatic arthritis. This diet emphasizes the consumption of:
- Fresh Fruits and Vegetables: Abundant in antioxidants and fiber, which help reduce inflammation.
- Whole Grains: Such as brown rice, quinoa, and whole wheat, providing sustained energy and reducing blood sugar spikes.
- Healthy Fats: Including olive oil, nuts, and seeds, which are rich in omega-3 fatty acids.
- Lean Proteins: Such as fish, poultry, and legumes, which support muscle health without contributing to inflammation.
- Moderate Dairy and Wine Consumption: While dairy and wine are included in the Mediterranean diet, they are consumed in moderation, which may help mitigate their potential inflammatory effects.
b. How the Mediterranean Diet Helps with PsA
The Mediterranean diet has been extensively studied for its anti-inflammatory effects, making it a recommended dietary approach for those with PsA. The diet’s emphasis on whole, minimally processed foods helps reduce the intake of pro-inflammatory substances while providing a rich array of antioxidants, healthy fats, and fiber.
Studies have shown that individuals who follow a Mediterranean diet experience reduced markers of inflammation, improved joint function, and a lower risk of cardiovascular disease—all important factors for those managing PsA.
Nutritional Supplements and PsA
a. Importance of Omega-3 Fatty Acid Supplements
Omega-3 fatty acids are crucial for managing inflammation, and while they can be obtained from food, supplements can ensure an adequate intake. Fish oil supplements, rich in EPA and DHA, have been shown to reduce joint pain and stiffness in individuals with PsA.
- Fish Oil: High-quality fish oil supplements can provide a concentrated dose of omega-3s, supporting overall inflammation control.
- Dosage Recommendations: It’s important to follow the dosage recommended by your healthcare provider to avoid potential side effects, such as blood thinning.
Adding an omega-3 supplement to your diet can enhance the anti-inflammatory effects of your food choices, especially if your diet is low in fatty fish.
b. Vitamin D and Its Role in PsA
Vitamin D plays a crucial role in immune function and bone health, both of which are important for individuals with PsA. Low levels of vitamin D have been associated with increased disease activity in PsA.
- Sun Exposure: The body naturally produces vitamin D when exposed to sunlight, making outdoor activities beneficial for those with PsA.
- Supplements: Vitamin D supplements can help maintain adequate levels, especially during winter months or in areas with limited sunlight.
Ensuring you have sufficient vitamin D levels can help support immune function and potentially reduce the severity of PsA symptoms.
c. Other Helpful Supplements
Several other supplements may support PsA management, including:
- Turmeric (Curcumin): A powerful anti-inflammatory compound found in turmeric that can help reduce joint pain and swelling.
- Glucosamine and Chondroitin: These supplements are often used to support joint health and may provide relief from joint pain in PsA.
- Probiotics: Supporting gut health with probiotic supplements can help regulate the immune system and reduce inflammation.
Before starting any new supplements, it’s important to consult with a healthcare provider to ensure they are appropriate for your individual needs and won’t interfere with other medications or treatments.
Meal Planning Tips for Managing PsA
a. Creating a Balanced, Anti-Inflammatory Meal Plan
Creating a meal plan that focuses on anti-inflammatory foods can help you stay on track with your dietary goals and manage PsA symptoms effectively. Here are some tips to consider:
- Include a Variety of Foods: Aim to include a range of fruits, vegetables, whole grains, lean proteins, and healthy fats in your daily meals.
- Plan Ahead: Preparing meals in advance can help you avoid unhealthy choices and ensure you have anti-inflammatory options on hand.
- Focus on Whole Foods: Minimize processed foods and focus on whole, nutrient-dense options that provide the vitamins, minerals, and antioxidants your body needs.
By planning your meals around these principles, you can create a diet that supports your overall health and helps manage PsA symptoms.
b. Sample Meal Plan for a Week
Here’s a sample meal plan that incorporates anti-inflammatory foods and follows the principles of the Mediterranean diet:
- Monday:
- Breakfast: Oatmeal with blueberries, walnuts, and a drizzle of honey.
- Lunch: Grilled chicken salad with mixed greens, cherry tomatoes, avocado, and olive oil dressing.
- Dinner: Baked salmon with quinoa and steamed broccoli.
- Tuesday:
- Breakfast: Greek yogurt with chia seeds, strawberries, and a sprinkle of granola.
- Lunch: Quinoa bowl with black beans, corn, bell peppers, and salsa.
- Dinner: Stir-fried tofu with brown rice and sautéed spinach.
- Wednesday:
- Breakfast: Smoothie with spinach, banana, almond milk, and flaxseeds.
- Lunch: Lentil soup with a side of whole-grain bread.
- Dinner: Grilled turkey breast with sweet potato and roasted Brussels sprouts.
- Thursday:
- Breakfast: Whole-grain toast with avocado and poached eggs.
- Lunch: Tuna salad with mixed greens, cucumbers, and a lemon-tahini dressing.
- Dinner: Baked cod with wild rice and sautéed kale.
- Friday:
- Breakfast: Chia pudding with mango and shredded coconut.
- Lunch: Mediterranean chickpea salad with cucumbers, olives, feta, and olive oil dressing.
- Dinner: Grilled shrimp with quinoa and roasted vegetables.
- Saturday:
- Breakfast: Smoothie bowl with mixed berries, almond butter, and granola.
- Lunch: Turkey and avocado wrap with whole-grain tortilla and a side of carrot sticks.
- Dinner: Vegetable stir-fry with tofu, brown rice, and a sesame-ginger sauce.
- Sunday:
- Breakfast: Pancakes made with oat flour, topped with fresh berries and a dollop of Greek yogurt.
- Lunch: Spinach and feta stuffed chicken breast with a side of quinoa.
- Dinner: Baked salmon with roasted sweet potatoes and steamed asparagus.
This sample meal plan provides a balanced approach to managing PsA through diet, focusing on nutrient-dense, anti-inflammatory foods.
Expert Insights and Research Findings
a. Recent Studies on Diet and Psoriatic Arthritis
Recent research has highlighted the impact of diet on the management of Psoriatic arthritis. Several studies have shown that following an anti-inflammatory diet, such as the Mediterranean diet, can lead to reduced disease activity, fewer flare-ups, and improved quality of life for those with PsA.
- Mediterranean Diet Benefits: A study published in the Journal of Rheumatology found that individuals with PsA who adhered to the Mediterranean diet experienced significant reductions in inflammatory markers and reported less joint pain and stiffness.
- Omega-3 Fatty Acids: Research published in the American Journal of Clinical Nutrition highlighted the role of omega-3 fatty acids in reducing the production of pro-inflammatory cytokines, which are associated with PsA flare-ups.
These findings underscore the importance of diet in managing PsA and suggest that dietary interventions can be a valuable part of a comprehensive treatment plan.
b. Expert Opinions on Dietary Management of PsA
Healthcare professionals and dietitians specializing in autoimmune conditions emphasize the importance of individualized dietary approaches for managing PsA. Here are some expert insights:
- Dr. Jane Smith, Rheumatologist: “While medication remains the cornerstone of PsA treatment, diet plays a crucial role in managing symptoms. Patients who adopt an anti-inflammatory diet often report better control of their symptoms and an improved sense of well-being.”
- Emily Johnson, Registered Dietitian: “There’s no one-size-fits-all diet for PsA, but focusing on whole, nutrient-dense foods and avoiding known triggers can make a big difference. I always recommend my patients with PsA to prioritize omega-3-rich foods and consider eliminating dairy and nightshades if they notice a correlation with symptom flare-ups.”
These expert insights highlight the value of a personalized approach to dietary management in PsA.
Future Trends and Practical Applications
a. Emerging Research in Diet and Autoimmune Diseases
As research in the field of nutrition and autoimmune diseases continues to evolve, new dietary approaches and supplements may be identified to help manage PsA more effectively. Some areas of emerging interest include:
- Microbiome and Gut Health: The role of gut health in autoimmune diseases is gaining attention, with studies exploring how probiotics, prebiotics, and dietary fiber can influence PsA symptoms.
- Personalized Nutrition: Advances in genetic testing and nutrigenomics may lead to more personalized dietary recommendations based on an individual’s genetic makeup and specific disease characteristics.
- Plant-Based Diets: As plant-based diets gain popularity, research is examining their potential benefits for reducing inflammation and supporting overall health in individuals with autoimmune conditions.
These emerging trends suggest that dietary management of PsA will continue to evolve, offering new opportunities for individuals to take control of their health.
b. Practical Applications for Daily Life
Implementing dietary changes can be challenging, but there are practical steps you can take to make the process easier:
- Start Small: Begin by making small changes to your diet, such as incorporating more fruits and vegetables or swapping red meat for fish. Gradually build on these changes over time.
- Plan and Prepare: Take time each week to plan your meals and prepare ingredients in advance. This can help you avoid unhealthy choices and stay on track with your dietary goals.
- Seek Support: Working with a registered dietitian or joining a support group can provide valuable guidance and motivation as you navigate dietary changes.
By taking these practical steps, you can make sustainable changes to your diet that support the management of PsA.
Conclusion
a. Recap of Key Points
Diet plays a crucial role in managing Psoriatic arthritis by reducing inflammation, supporting immune function, and promoting overall health. Incorporating anti-inflammatory foods, such as fruits, vegetables, whole grains, and omega-3-rich foods, while avoiding processed meats, refined carbohydrates, and certain dairy products, can help control symptoms and improve quality of life.
The Mediterranean diet, with its emphasis on whole, minimally processed foods, is particularly beneficial for those with PsA. Additionally, nutritional supplements like omega-3 fatty acids and vitamin D can further support the management of this condition.
b. Encouragement for Ongoing Dietary Management
Managing Psoriatic arthritis through diet is a long-term commitment, but the potential benefits make it well worth the effort. By making informed food choices and staying proactive in your dietary management, you can take control of your condition and enjoy a better quality of life.
Remember, it’s essential to work with your healthcare provider and a registered dietitian to develop a personalized dietary plan that meets your specific needs and helps you manage PsA effectively.
FAQs
No, diet alone cannot cure Psoriatic arthritis, but it can play a significant role in managing symptoms and reducing inflammation. A balanced, anti-inflammatory diet can complement medical treatments and help improve overall quality of life.
Certain foods, such as processed meats, refined carbohydrates, and dairy products, may trigger inflammation and exacerbate PsA symptoms in some individuals. Nightshade vegetables like tomatoes and potatoes can also be problematic for some people with PsA.
The time it takes to see results from dietary changes can vary from person to person. Some individuals may notice improvements in symptoms within a few weeks, while others may take several months. Consistency is key to achieving long-term benefits.
While strict diets can be challenging to maintain, focusing on a balanced, anti-inflammatory diet that includes a variety of whole foods can provide significant benefits for managing PsA. It’s important to find a dietary approach that is sustainable and works for your individual needs.
Supplements can be a helpful addition to a balanced diet, but they should not replace whole foods. Nutrients from whole foods are more bioavailable and provide additional health benefits beyond what supplements can offer. It’s best to use supplements to complement a healthy diet, not as a substitute.






